If you experience leg pain or numbness, it’s not always just a muscle ache. It may be a sign of peripheral artery disease (PAD), a common circulatory problem caused by plaque buildup in the arteries of your legs.
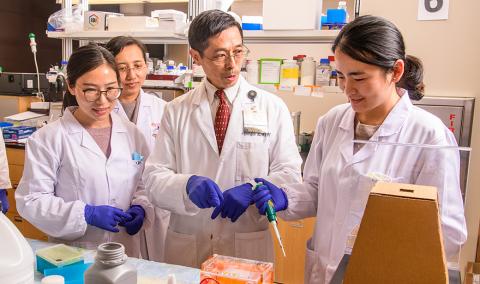
At University of Missouri Health Care, our expert cardiologists and vascular surgeons work together to provide personalized diagnosis and treatment of PAD. As a patient at an academic health center like MU Health Care, you benefit from a multidisciplinary team approach and the latest treatments for PAD. Our physicians are active in research, using the latest medical evidence to guide your care.
Peripheral artery disease symptoms and risk factors
People who smoke or have diabetes are at especially high risk for peripheral artery disease. If you have risk factors for PAD, a screening can help determine if you have the disease.
Risk factors include:
- Aging
- Cigarette smoking
- Diabetes
- High blood pressure
- High cholesterol
- Obesity
- Personal or family history of PAD, cardiovascular disease or stroke
- Physical inactivity
Symptoms of PAD include:
- Cold feet
- Feet or leg wounds that heal slowly
- Leg numbness
- Leg pain
- Pain or cramping in your legs when walking
- Poor toenail or hair growth on your legs and feet
If you have risk factors or symptoms, your physician may suggest you have a screening for PAD. Ultrasound technology screenings examine the veins and arteries in the legs to look for plaque buildup. The screenings are painless, noninvasive and only take a few minutes.
Advanced diagnosis and treatment of peripheral artery disease
In serious cases of peripheral artery disease, tissues in your legs or feet may die because they don’t get enough oxygen. If this occurs, you may need an amputation to remove part of your leg or foot. Amputating a leg is a difficult decision that is made by more than 100,000 PAD patients each year.
However, with early detection and treatment, you can avoid amputation. At MU Health Care, we offer preventive screening services and comprehensive treatments to improve your blood flow and artery health. Your treatment plan is personalized to you and may include:
Lifestyle changes
Lifestyle changes can slow down plaque buildup and help restore blood flow. Your physician can help you make these changes, which might include quitting smoking, exercising and improving your diet.
Medicines
Your physician may prescribe medicine to manage problems that make PAD worse. You may need blood pressure medicine, cholesterol-lowering medicines or blood thinners to prevent blood clots.
Minimally invasive procedures
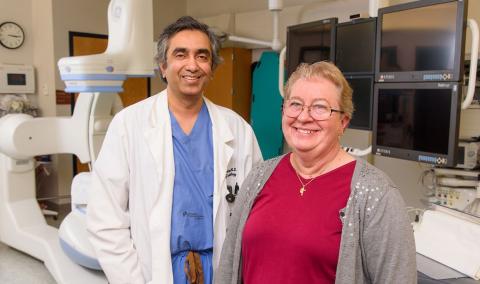
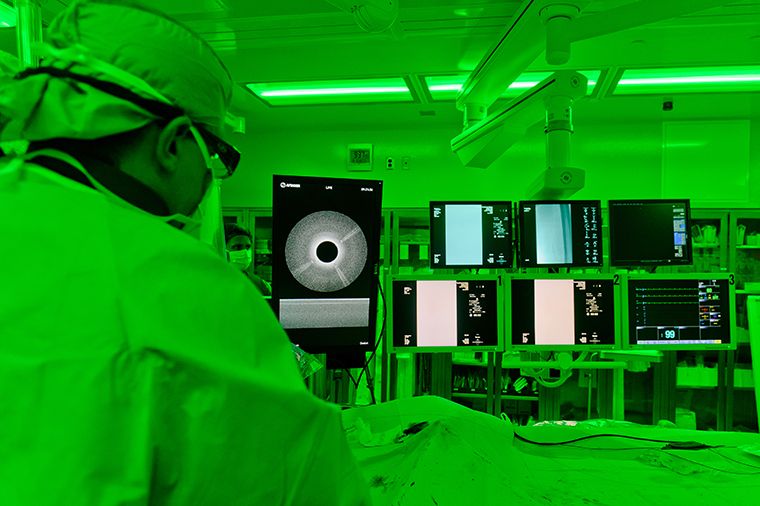
At MU Health Care, we provide the latest minimally invasive procedures to open arteries and restore blood flow. For these procedures, your vascular surgeon uses just one incision to perform surgery. Physicians use X-rays during these procedures to guide a thin tube (catheter) through the incision and into the blocked artery.
Catheterization
Our physicians use a specialized catheter — an Ocelot catheter — that includes a camera on the end. Once the catheter is in place, your vascular surgeon can use a small drill-like tool at the end of the catheter to break through blockages in your artery, allowing more blood flow.
Your physician can also place a mesh wire tube, called a stent, that will hold the artery open in the future. Because it does not need fluoroscopy (X-ray imaging), the Ocelot catheter reduces your exposure to radiation and can break up large blockages that were once difficult to eliminate.
Percutaneous transmural arterial bypass
For patients who have a long, complex obstruction in their superficial femoral artery, MU Health Care offers an innovative and minimally invasive treatment to relieve muscle pain and other symptoms caused by reduced blood flow — called claudication.
During a percutaneous transmural arterial bypass (PTAB), your vascular surgeon and interventional cardiologist work together to bypass the blockage in your leg. Using a catheter guided by angiogram, they navigate to the site of the blockage and use a stent graft to create a new channel for oxygenated blood through part of the femoral vein, which runs next to the artery.
Patients who receive PTAB intervention are under anesthesia and can return home the day after their procedure. As a minimally invasive procedure, PTAB comes with some risks that your doctor will discuss with you before the procedure, but it is safer than an open procedure and results in less pain and shorter recovery times than previous treatments for blocked femoral arteries. Some patients do not need rehab after the procedure and can resume daily activities within a few days.
Learn more about Heart & Vascular Care at MU Health Care.
Related Conditions & Treatments
- Aortic Disease Care
- Atrial Fibrillation (AFib) and Arrhythmia
- Carotid Artery Disease
- Chest Pain
- Chronic Total Occlusion (CTO)
- Congenital Heart Disease
- Coronary Artery Disease
- Cardiothoracic Surgery
- ECMO Heart and Lung Life Support
- Heart Attack
- Congestive Heart Failure
- Heart Valve Disease
- Pediatric Cardiology
- Pediatric Vascular Anomalies
- Peripheral Artery Disease (PAD)
- Structural Heart Program
- Transcatheter Aortic Valve Replacement (TAVR)
- Vascular Surgery
- Women's Heart Health