Coughing was just a fact of life for Hannah Gryder.
For as long as her grandmother, Tina Wood, can remember, the rasping noise and chest spasms would disrupt Hannah’s sleep. She was diagnosed with asthma at five and got sick with pneumonia and bronchitis several times.
None of it stopped Hannah, who turned 12 in 2024, from smiling, finding joy in spending time at the lake in the summer or playing softball in the fall and spring. But it was clear to Hannah and Tina that something wasn’t right.
In their search for answers, they went to allergy specialists and tried allergy shots. Hannah had her tonsils and adenoids removed, hoping that would help. Tina even completely redecorated their home in Pleasant Hope, Missouri, outside of Springfield.
“We thought she might have been allergic to something in the carpets,” Tina said. “We tore out all the carpet, all the throw rugs, everything, and replaced it with hardwood floors. We changed all our bedding, repainted, trying everything we could to solve the problem.”
But Hannah’s cough persisted as she moved through middle school. She started seeing a pediatric pulmonologist in Springfield, who diagnosed her with a chronic lung condition called bronchiectasis. Hannah’s airway was thicker than normal because of extra mucus that made infections more common.
She was referred to MU Health Care’s Children’s Specialty Center, where testing from the cystic fibrosis team, including Rebekah Nevel, MD, confirmed that Hannah has cystic fibrosis.
“It sounds strange, but we were grateful to hear an answer,” Tina said. “We were so grateful to finally have a plan in place and to know that we were headed in a direction to get Hannah some health and healing.”
Cystic fibrosis, or CF, is a genetic condition that affects the body’s ability to regulate chloride salt in cells. Salt channels are how the body changes the amount of water in cells.
Less water means thicker, stickier mucus, which causes damage to lung tissue and makes airway infections more likely. CF can also lead to liver, gastrointestinal, pancreas and endocrine problems.
“Cystic fibrosis takes a team to care for it,” Nevel said. “As one of four CF centers in Missouri, we have everything in place to help pediatric patients, like Hannah, and adult patients prevent lung disease progression and live their lives to the fullest.”
Cystic fibrosis centers are accredited by the Cystic Fibrosis Foundation and recommend treatment based on the latest guidelines. Hannah’s team includes doctors, advanced practice providers, nurses, a respiratory therapist, dietitians and other care team members who help manage her complex condition.
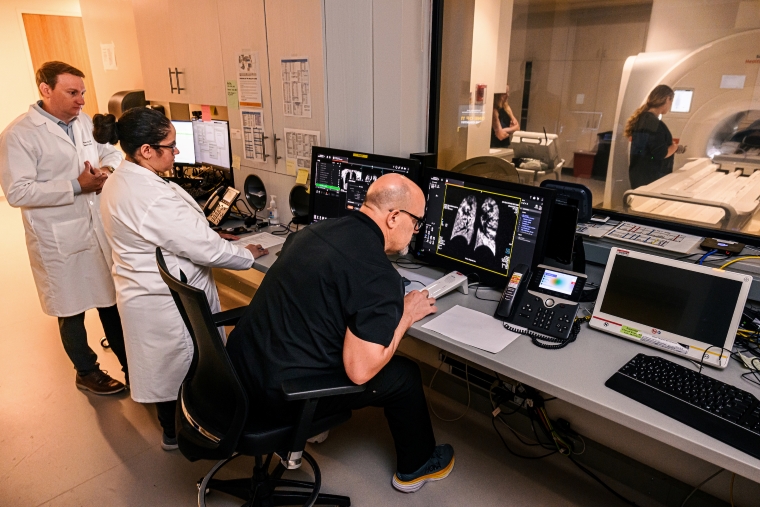
But Dr. Nevel, and everyone else involved in Hannah’s care, has access to something most CF centers do not. Steps away from her clinic, Dr. Nevel can walk into the Roy Blunt NextGen Precision Health building to get the clearest images possible of her patients’ lung function using an MRI machine and xenon gas.
Before this technology was developed by MU Health Care and School of Medicine researchers and radiologists Talissa Altes, MD, and Robby Thomen, PhD, pulmonologists were unable to use MRI to see a diagnostic image of lung function, relying on useful but imperfect tools like CT scans, spirometry and plethysmography.
“When I see Hannah’s lung obstruction on spirometry, all I can say is that there is obstruction,” Nevel said. “I can’t see where, or what, is being impacted. Xenon MRI shows us a picture of that. It also tells us which areas that might look less affected have difficulty with gas exchange.”
Research by Altes and Thomen showed that hyperpolarizing xenon aligned its atomic particles, to allow it to show up on MRI scans.
This FDA-approved clinical scan can show doctors at MU Health Care how healthy a person’s lung tissue is, and how efficient oxygen and carbon dioxide are exchanged in the lungs. Hannah was one of the first patients at MU Health Care to receive a xenon MRI scan for clinical care.
“Hannah’s results helped Dr. Nevel to suggest some medications that would help Hannah’s treatment because she could see more clearly the things that were going on in her lungs,” Tina said.
For Hannah, all it takes is a few regular breaths in. She inhales the nonreactive xenon, which is prepared seconds before, and holds the breath for about 20 seconds while the MRI machine runs. After a few minutes, she takes an inhaled medication, and then a few minutes later receives another MRI to check the effectiveness of that treatment.
On the other side of the glass, her doctors have immediate, detailed feedback on the health of her lungs.
“For someone like Hannah, who wasn’t diagnosed with cystic fibrosis when she was born, the benefit of xenon MRI is huge,” Nevel said. “That detailed evaluation allowed us to confidently fine-tune her treatments.”
At home, Hannah’s routine to get ready for school has lots of steps. She takes inhaled medications including albuterol, hypertonic saline, and other nebulized treatments such as inhaled antibiotics, and uses a vibrating vest that manually loosens the mucus in her airways.
“She has to wake up a little earlier,” Tina said. “It takes about an hour, but doing all these things means she has a normal school day. She’s not coughing as much, and she can breathe normally during PE.”
Hannah and her family have made a few trips to Columbia for the xenon MRI scans. But most of her ongoing cystic fibrosis care happens at MU Health Care’s cystic fibrosis outreach clinic in Springfield, much closer to home.
“Our patients and their families really appreciate the outreach clinic,” Nevel said. “It is a burden to drive long distances for regular visits. Hannah and her family come to Columbia for their bigger annual appointment, but they have access to a clinic that’s much closer for their follow-up care.”
For Hannah and the Wood family, that means more time spent together at softball games cheering on their star in left field. It means more time soaking up the sun and water at the lake, tubing and swimming with confidence.
“On our first visit, everyone was so personable and kind that we knew MU Health Care was the right place for Hannah,” Tina said. “I can’t describe the change we’ve seen in her since she started treatment. Everybody’s sleeping better because she’s coughing less. And all the doctors and everyone here remain optimistic for her. That helped us understand her diagnosis, but also just look at the positive things that are happening for her.”





