Vertebral body tethering, or VBT, has changed the way physicians think about surgical treatment of adolescent idiopathic scoliosis (AIS) for patients, their families, and for physicians like Daniel Hoernschemeyer, MD.
An orthopaedic surgeon at the University of Missouri Health Care, Hoernschemeyer has seen — and helped — the procedure advance from experimental to FDA approval under humanitarian device exemption. In tandem, the procedure itself has advanced because of several important factors.
“Specifically, improvement in patient selection has evolved into understanding the right indications,” Hoernschemeyer said. “This is not a procedure that is for everyone, but we know things now that we didn’t when I started placing tethers in 2013.”
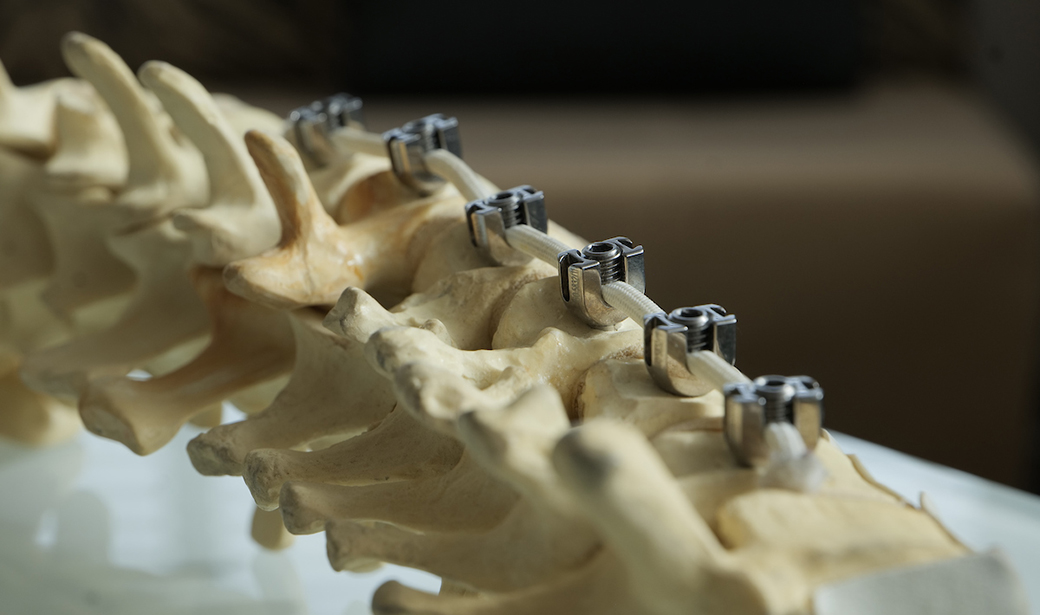
VBT is a fusionless treatment for AIS that modulates future spinal growth by mounting anchors for a braided polypropylene tether to the vertebral body along the convexity of the curve. Compressing the outside of the curve slows growth there, while tensioning the concavity stimulates growth on the inside of the curve, guiding the spine into an upright position.
Because it requires at least two years of future growth, screening patients for skeletal maturity is a key step in patient selection. Adolescents with a Cobb angle of between 40 and 65 degrees who are not yet skeletally mature are candidates. Similarly, adolescents with Sanders Maturity Scale of 1 or 2 who are experiencing a Cobb angle of at least 25 degrees are very likely to see their AIS progress beyond bracing to necessitate surgical intervention. Patients with spinal rigidity or closed growth plates are not candidates for VBT.
“Early in the process, studies showed a success rate of about 59%, but our patients here have a success rate of 75-80%, and I think tightening our criteria accounts for our successful data,” Hoernschemeyer said.
Another major improvement has come from familiarity with access and placement of hardware thoracoscopically. Developing a team approach that starts with preoperative bloodwork ensures anesthesia and single-lung ventilation are delivered smoothly, and using a lateral decubitus approach gives the surgical team ideal access to the spine.
“Our access has gotten better, quicker, which means the procedure has gotten increasingly faster and better,” Hoernschemeyer said. “We can now perform the procedure in four or five hours. Our first procedures were much longer, almost double that amount of time.”
Less time in the operating room and better efficiency in surgical access has also improved patient pain levels as they wake up. Adolescents no longer need to be discharged into pediatric intensive care units or use patient-controlled anesthesia (PCA).
“We take extra steps like closing the pleura over the hardware when we’re done so that we can pull the chest tube on Day 1,” Hoernschemeyer said. “With better definition of pain management, we postoperatively no longer need a PCA or heavy narcotics, which means most of our patients are discharged on post-op Day 2.”
All together VBT gives patients a treatment for AIS that does not require spinal fusion in 90-95% of cases, preserving their anatomy and flexibility. It also gives kids active in sports a faster return to activity — three months, compared to six for fusion patients — and 95% return to some level of activity following VBT.
“Seeing something that didn’t exist when I was training that now offers this level of care for kids is amazing,” Hoernschemeyer said. “Treatments like this are revolutionizing care for kids, and it feels special to be part of that.”